Inflammation — does our diet foster a hero or a villain?
For the past few years along-side my clinical work I have been a scientific researcher at the Stress, Psychiatry and Immunology (SPI) Lab at Kings College London, helping to expand our understanding of the mechanisms, at the level of the body and the brain, underlying the effect of nutrition on mental health. Especially in the crucial early years!

WHAT DO WE KNOW SO FAR?
Let’s start with inflammation, you have probably all heard of and experienced inflammation in some form. Like when a wound swells up, turns red, and hurts — that’s inflammation! It is a physiological response to cellular and tissue damage, designed to protect the host from bacteria, viruses, and infections by eliminating the bad guys (pathogens), promoting cellular repair, and restoring balance internally — our internal hero!
However, a prolonged inflammatory state termed by scientists as chronic low-grade inflammation that persists day in and day out has the opposite effect — including irreparable damage to tissues and organs, and increased risk of disease status — our internal villain…
Interestingly, science has started to show that there is a precise biological mechanism that links the physical response to inflammation, to a behavioral response — in other words, it also affects our mental health.
HOW DOES THE IMMUNE SYSTEM AFFECT THE BRAIN?
When an inflammatory response is triggered, a series of proteins , known as the inflammatory cytokines, are released into the blood stream and tissues. They act like messengers between different organs, urging the body to fight the infection.
What scientists have now shown is that inflammatory cytokines can also reach the brain and affect some crucial cellular processes involved in mood and behaviour regulation.
Animal studies have shown that cytokines can reach the brain via the blood-brain barrier (BBB), a border of cells protecting the brain against circulating toxins while at the same time, allowing vital nutrients and other substances to pass.
So, in its villainous role, inflammation can go from the body to the brain and has been established as a risk factor for several neuropsychiatric disorders such as ADHD, depression, and schizophrenia, including in children and adolescents.

Interestingly, this presents an opportunity! Inflammation is therefore an important therapeutic target to study. But what causes our hero to turn into a villain? What triggers a state of chronic low-grade inflammation in children and adolescents?
Well, the potential factors are diverse. Stressors such as trauma through adverse childhood experiences, psychosocial stress, as well as modifiable lifestyle sources such as limited physical exercise or smoking are all capable of evoking a deleterious inflammatory response.
So then, can diet?
Overall, it is well established that a healthy diet in childhood and adolescence is crucial for physical health including optimal growth and development and for disease prevention. In terms of mental health, scientists are also starting to show associations between a higher quality dietary intake and a reduced risk of adverse mental health outcomes in both children and adolescents.
However, many questions remain unanswered. Including, why and how dietary pattern intake and/or specific nutrients can exert a positive or negative effect on mental health outcomes, and why these effects are stronger in some people than in others. To answer these questions we need an understanding of the key biological mechanisms underpinning these pathways.
Bringing it all together, since we know that inflammation can influence mental health, and dietary intake is associated with mental health — is the missing link in the biological pathway inflammation?
Does dietary intake influence inflammation in children and adolescents? And if so, how?

Potential pathway whereby dietary intake can affect mental health.
(Source: authors own work)
WHERE TO NEXT?
I recently conducted and published a systematic review — essentially seeking out all available, existing research on a topic that we want to learn more about and distilling it down to some key findings. The literature is selected and studied collectively with pre-specified criteria in mind. This helps us to identify patterns, similarities, and differences in the findings and then draw conclusions and derive new hypotheses for future study directions.
After an intense process of sifting through 10,611 (to be precise!) potential scientific papers we whittled down the relevant body of literature that fit our criteria to 53 papers and set about teasing out the key messages.
WHAT DID WE LEARN?
You can read the full breadth of my findings in the systematic review, which is in fact the first systematic review to be published that examines dietary intake and biological markers of inflammation in both children and adolescents.
Before we continue, you might be asking what are biological markers of inflammation? Briefly, these markers, including C-reactive protein (CRP) and cytokines analyzed from blood samples circulate in the body when inflammation is triggered. These small proteins are messengers released to inform the body an infection needs fighting, they are important signaling molecules in the immune response — our hero! For scientists, they are an important indication of levels of inflammation. An over-production of cytokines is indicative of a pro-inflammatory state through chronic low-grade inflammation, which can have deleterious results including irreparable damage to tissues and organs, and increased risk of diseased states. Our villain!
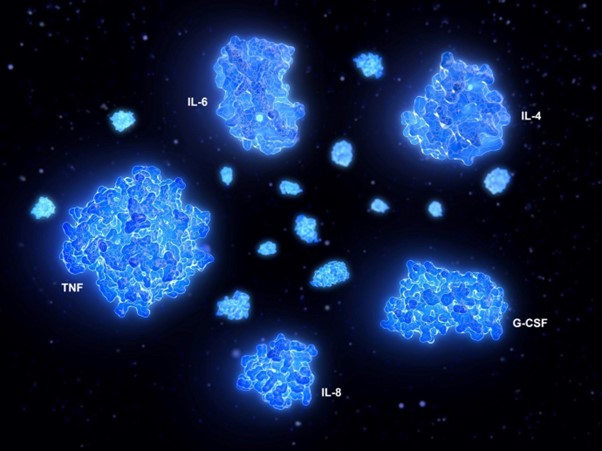
A cytokine storm is a physiological reaction in which the innate immune system causes an uncontrolled and excessive release of pro-inflammatory signalling molecules called cytokines.
(Source: Pexels)
So what did I find in the research with regards to dietary intake and inflammation in children and adolescents — does it foster the hero or the villain?
Certainly, healthy dietary patterns of high quality, such as adherence to a Mediterranean Diet, rich in vegetables, fruit, whole grains, legumes, nuts, fish, and low-fat dairy, coupled with low intakes of red meat and adequate intakes of healthy fats such as omega-3 polyunsaturated fatty acids (omega-3 PUFA’s which you might know as “fish oil”), has been shown to reduce systemic inflammation. As well, studies that had examined the individual constituents of such healthful patterns separately including vegetables and fruit, healthy fats like omega-3 polyunsaturated fatty acids (PUFAs) or vitamins C and E also showed positive results, whereby high intakes of these individual constituents were associated with decreased levels of circulating inflammatory biomarkers.
In fact, research from the lab I worked in at Kings College has demonstrated omega-3 PUFAs, regulate the immune response by inhibiting the activation of pro-inflammatory pathways and reducing cytokine expression. Other studies have also demonstrated intake of a high-dose eicosapentaenoic acid (an omega-3 fatty acid) improves cognitive symptoms (symptoms associated with impaired memory and learning) in Attention Deficit Hyperactivity Disorder (ADHD) youth that have lower than optimal levels of EPA evident in their blood. Lastly, our research in animal models has demonstrated inflammation-induced reductions in neurogenesis (production of neurons) can be prevented through omega-3 PUFAs intake.
SEEMS DIET FOSTERS THE HERO?
Not so fast, it can also foster the villain…
In contrast to a healthful dietary pattern, the Western dietary pattern which is comprised of high intakes of ultra-processed foods like potato chips, cakes, and sweetened breakfast cereals, sodium (salt), and foods that contain trans- and saturated fatty acids like fried fast foods elicits a pro-inflammatory response and increases levels of circulating inflammatory biomarkers.

Similarly, across the studies included in my review that examined the Dietary Inflammatory Index (DII), a tool that assesses the inflammatory potential of a diet, I found that diets with high inflammatory potential (a higher score in the DII), inducing a higher inflammatory response, increased pro-inflammatory biomarkers.
Indeed, even mild undernutrition through poor quality diets has far-reaching mental, physical and social problems in children and adolescents, with overall effects that can last two to three generations.
WHAT DOES ALL THIS MEAN?
Well, in children and adolescents a good quality diet, high in vegetable and fruit intake, whole grains, fiber, and healthy fats is essential for optimal growth, development, and the amelioration of low-grade inflammation — aka, fosters our inner hero!
Further, modifying dietary intake as early as during childhood and adolescence to encompass high quality, nutrient-dense foods represents an important and promising therapeutic strategy in order to maintain a regular immune response and to reduce the risk of adverse mental health disorders and associated co- and multi-morbid conditions later in life.

Related posts
Tinnitus Awareness Week – 6th to 12th February, 2023
What Is Tinnitus? Tinnitus is the perception of sound in the absence of external sound.…
Appointment Procedure during CV-19
Updated 15th May We are now able to offer Emergency / Urgent / In need…
Functional Fitness
Functional fitness is exercise that mimics everyday movement and activity that improves your ability to…
50 YEARS AT SPRINGBANK HOUSE
Richard Pitcairn-Knowles was practising Osteopathy locally in the late 50s when he decided that he…

